Just as physical injury claims that rely heavily on pharmacological modalities to address the symptoms of pain without active therapies to promote functional recovery should raise flags, mental–only claims that fail to incorporate a psychotherapy component should raise concerns that the patient’s PTSD is not being adequately or effectively treated.
Common benzodiazepines: alprazolam, diazepam, and lorazepam
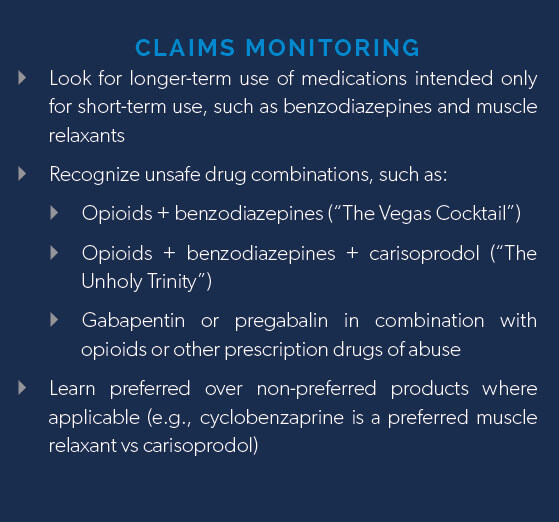
Benzodiazepines are not meant to be taken chronically. Long-term adverse effects associated with benzodiazepines include cognitive impairment, physical dependence and withdraw, an increase in anxiety and depression, overdose, and death.
Additionally, even though evidence-based guidelines warn against combining benzodiazepines and prescription pain medications, benzodiazepines are almost always prescribed in combination with opioids in workers’ comp, despite significant risks.2

Muscle relaxants are frequently used in workers’ comp to alleviate muscle spasms, pain, and overresponsive reflexes. While muscle relaxants can help with pain, they are not meant to be taken chronically as overreliance can lead to dependence and withdrawal, fueling abuse.
Common muscle relaxants: cyclobenzaprine, carisoprodol, methocarbamol, and tizanidine
Muscle relaxants should be used with caution, as they present the risk of adverse effects such as mood changes, impaired thinking, paralysis, CNS depression, respiratory depression, and heart failure.
Risk varies among products. Carisoprodol (Soma®) is known for having more severe withdrawal symptoms than cyclobenzaprine, increasing its risk for abuse. From 2004-2009, emergency department visits involving carisoprodol doubled from 16,000 to 32,000.5
While muscle relaxants can be abused by themselves, as depressants they can be more dangerous when combined with other depressants, such as alcohol, benzodiazepines, and opioids, increasing the likelihood of potentially fatal adverse effects.
Gabapentin and pregabalin are anticonvulsants (anti-seizure drugs) often used off-label for the treatment of certain types of neuropathic pain. While these drugs are considered very safe by themselves, they do have mood-altering properties and can be abused to boost the high of other drugs of abuse.
The excessive ingestion of gabapentin or pregabalin significantly increases risk for suicidal thoughts and overdose, a cause for concern as these drugs are seeing rising levels of abuse to boost the euphoric high of opioids.
The state of Kentucky recently classified gabapentin as a Schedule V drug,8 while Ohio and Massachusetts now require the dispensing of gabapentin to be reported to their respective prescription drug monitoring programs.9-10
In the event assistance is required analyzing a patient’s drug regimen, Healthesystems’ clinical pharmacists are available to answer questions for our customers and pharmacists within our network. Please contact our Ask a Pharmacist Drug Line at 866.646.2828. Questions can also be submitted online at www.healthesystems.com, or emailed to DrugInformation@Healthesytems.com