Older workers represent the fastest-growing portion of the workforce. The Bureau of Labor Statistics reports that approximately 40% of individuals 55 or older are working or actively looking for work. In the next decade, 1 out of 4 workers will be aged 55 or older, with the proportion of workers aged 65 or older representing the highest growth rates.1 In addition, this group of workers is increasingly holding full-time positions, a trend that has continued over the last two decades.2
The aging demographic of the workforce naturally brings with it considerations for workplace safety, as well as differences in injury and treatment when compared with younger counterparts. While older employees overall sustain relatively fewer injuries than younger age groups, it varies depending upon occupational demand. Injuries sustained by older workers tend to be more severe,2 more costly, and result in more time away from work.3 Some of this can be attributed to natural biologic aging processes, such as reduced muscle mass and recovery abilities, but there are additional medication-related and comorbidity concerns that must also be considered for optimal management.
From a pharmacy perspective, there are specific medication-related considerations for optimal management of the older patient population. For example, certain medications that may be appropriate to prescribe for a 40-year-old may not be equally as appropriate for a 65-year-old with a similar injury, or may come with additional precautions or different dosing recommendations.
The reason? There are biologic changes that occur as we age that alter how our bodies metabolize and react to medications.
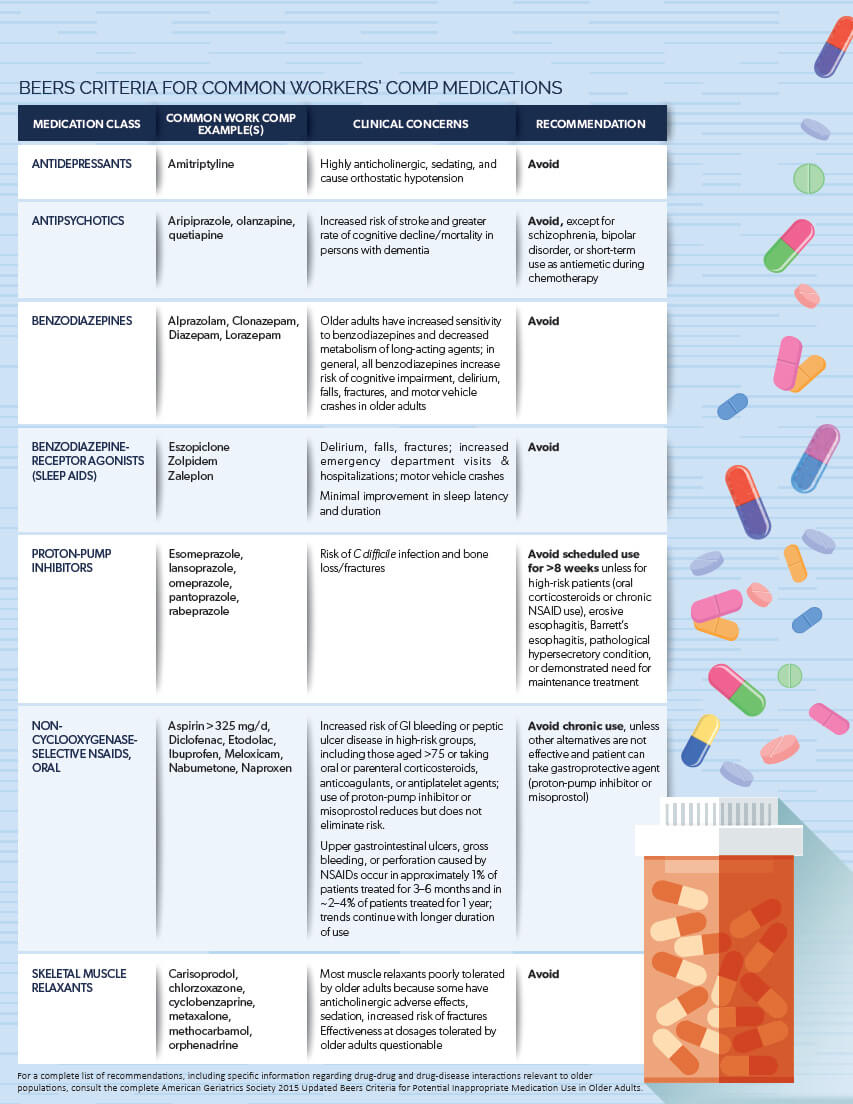
The Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, commonly called the Beers List or Beers Criteria, are guidelines published by the American Geriatrics Society to help discourage the prescribing of inappropriate medications in older adults. While the Beers Criteria are largely targeted at populations 65+, there are other considerations included, such as certain diseases or syndromes that may also have prescribing implications. The Beers Criteria are not specific to treatment of injured workers; however, there are a number of medications included in the Beers Criteria that apply to workers’ compensation populations.
Below is a list of medications commonly prescribed in workers’ compensation that are potentially inappropriate for older adults, extrapolated from the Beers Criteria.4,5
While there are specific considerations related to the management of older worker populations, a patient cannot be assessed according to age alone, but rather upon the totality of overall health.
The prevalence of comorbid conditions in older individuals plays a significant role in these workers’ ability to recover, the choices made in their care management, and the medical costs associated with the claim.
Ultimately, individual health risk factors are a more significant driver of healthcare costs than older age alone. An assessment of workers aged 19-34 with five or more risk factors for chronic disease revlealed significantly higher medical costs compared with workers aged 65-74 with few or no risk factors.6
The presence of multiple chronic conditions is increasing among all age groups – 1 out of 4 adults in the United States were reported to have more than one chronic condition in 2014.9 This has a significant impact on healthcare utilization and costs regardless of age. Workers’ compensation claims in which the patient has been diagnosed with a single comorbidity are approximately twice the cost of comparable claims,8 and individuals with multiple conditions incur higher healthcare costs yet.
Thus while general trends provide parameters for managing older patients on a population level, individual risk factors must also be considered for optimal patient management.

Older patients are more likely to be prescribed multiple prescriptions for long-term durations. A large portion of older adults also use over-the-counter medications and dietary supplements, which aren’t visible within a claim. These scenarios increase the risk that polypharmacy (multiple concurrent medications) may occur or go unnoticed.
A number of drugs are contraindicated in the older population due to increased propensity for side effects. Other drugs may require special considerations or dosage adjustments. Medications that are inappropriate for older patients due to increased risk for side effects are included in the Beers Criteria.
A medication dosing schedule for a patient who is 30 years old may not be appropriate for a patient who is 60 years old due to changes in drug metabolism that occur as a person ages.
Older patients may experience cognitive decline, which could lead to forgetting to take medications (nonadherence), taking medications too often (misuse), or irregular refills.